In recent years, we have been exploring digital technologies that can expand our capabilities, simplifying clinical procedures and improving our treatment plans thanks to higher-quality diagnoses and operational protocols .
However, the issue of choosing the type, number, and position of implant devices during the design phase remains a matter of exclusive clinical expertise, as well as highly subjective. In this context, biomechanics plays an important yet still little-known role, due to failures or problems that manifest early due to immediate loading, and prosthetic issues that arise following the application of rehabilitation.
In these cases, there are many factors to consider, often influenced by the subjective characteristics of the patients being rehabilitated.
Certainly, we all observe the patient's "biotype", however, we often do not translate these evaluations into physical/mechanical considerations.
Age and gender can influence our choices, just as it is important to examine the tone of the masticatory muscles . In addition to these characteristics, it is necessary to perform a thorough intraoral assessment , along with a check for the presence of teeth in the same arch to be rehabilitated, with the resulting proprioceptive considerations and the participation of healthy teeth distally in our project. All these steps allow us to provide the nervous system with different information about chewing, from the replacement of all the teeth in a half-arch; the situation is even more complex in a fully implant-supported rehabilitation.
The decision-making process is influenced by the residual condition of the opposing arch— which is opposed to the prosthesis we will be placing—the number of teeth, the periodontal situation, and morphological aspects that may reveal previous parafunctions or masticatory overload. All of this is done with a view to possible future modifications, such as switching from a complete denture (a convenient opponent to our rehabilitation) to an implant-supported fixed prosthesis.
Figure 1: clinical situation of partial upper edentulism and complete lower dental formula
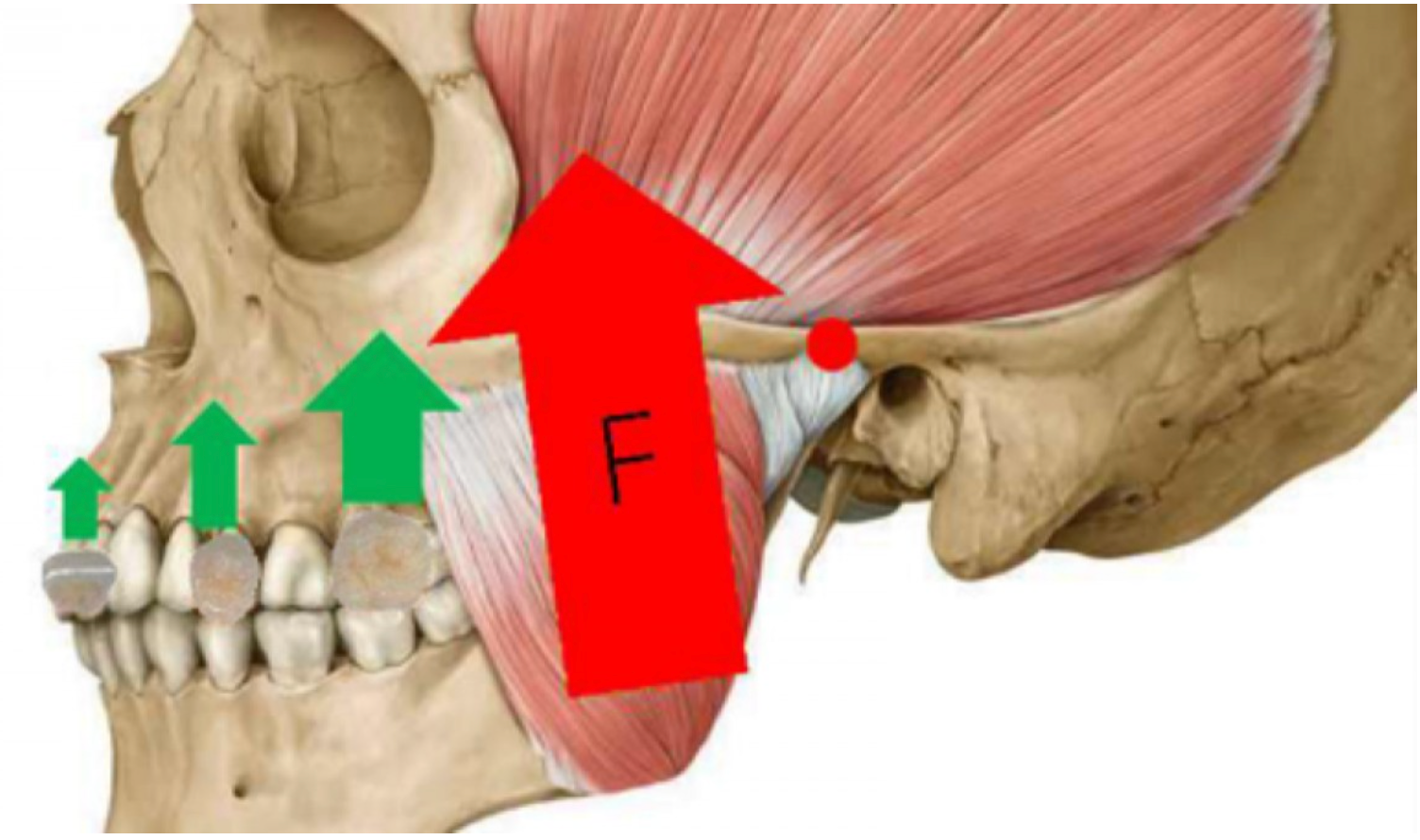
Teeth to be replaced in implant-prosthetic rehabilitation perform different functions, and their simple observation requires in-depth considerations. Simply observing the root support of a canine and a posterior incisor is enough to understand their different functional requirements: one is designed to withstand tangential loads, and the other to dissipate orthogonal forces. The implant design must take these needs into account, otherwise the peri-implant bone may suffer, or in more unfortunate cases, the implants themselves may become loose or fracture. Conversely, an upper lateral incisor or lower central incisors have inferior root development, as a result of their position and distance from the point of application of the masticatory force and the fulcrum of mastication (class III lever).
Figure 2 : Point of application of forces and position of resistance within the stomatognathic system
This consideration is directly related to the size of the implant we plan to insert, which should therefore not only depend on the bone availability of the recipient site, but should also be highly dependent on the direct and indirect stress the implant will experience during chewing, both during immediate loading and after osseointegration. Further considerations may be necessary if multiple implants are planned, either independent or joined together.
Figure 3 : Analysis of bone availability with the aid of CBCT, choice of some B1ONE devices with reduced diameter but compensation with an increase in number: programming with favorable load distribution axes
It's worth remembering that tilted implants function perfectly when placed in a number and position that maximizes their position. Creating an unfavorable angle between the prosthetic restoration, the occlusal load, and the implant device, however, represents an extremely high biomechanical risk for both the recipient tissue and the integrity of the device.
Another interesting aspect to consider is the choice and understanding of the materials available for prosthetic rehabilitation. This choice is influenced by economic considerations and the previously discussed considerations regarding: biotype, position in the oral cavity, dimensions of the implant device, any reciprocal connections, and the relationship with the antagonist. The rigidity of the chosen material represents an advantage when considering the maintenance of the results achieved over time (occlusal stability) and a disadvantage when, if not properly controlled, it transfers occlusal stress to the device and its components.
Figure 4: lower overdenture: prosthetic design appropriate to the availability of implant support
Paradoxically, Patients who can be monitored frequently and regularly can be rehabilitated with any material Because any corrections due to physiological changes in our dental morphology and chewing can be detected early and corrected before they become traumatic. Conversely, if we suspect we're unable to perform frequent chewing reassessments, it may be advisable to use materials that can adapt to the evolution of our chewing dynamics.
The choice of prosthetic device, whether screw-retained or cemented, is not directly related to biomechanical aspects. The former is particularly complex due to its passive management, however, when performed perfectly, it is versatile and easily removable, even for routine and emergency maintenance. Cemented prostheses present the well-known problem of imperfect removal of the cementing material, although they are mistakenly considered simpler because they are similar in protocol to those for prosthetics made on natural teeth.
Rarely does the failure to consider just one of these aspects lead to a serious or irreversible problem, however, often, when observing a critical situation, the combination of multiple factors unfortunately turns out to be responsible for failures unrelated to biological or inflammatory aspects.
Implant-prosthetic planning based solely on a radiological examination is often insufficient. Even more so, it seems insufficient to standardize treatment plans and, if this method is used (for example, a rehabilitation with four lower implants with the two distal ones tilted), develop the plan by considering the use of osseointegrable devices with dimensions and positioning that fully satisfy the biomechanical requirements and meet the requirements outlined.
Work by Dr. Paolo Arosio







Share: