THE MONOPHASIC SYSTEM WITH THE VERSATILITY OF A BIPHASIC SYSTEM
Digital workflow currently represents the most advanced solution for the design and implementation of implant-prosthetic rehabilitations.
Patient virtualization begins with a TRIOS 3Shape intraoral scan and matching with 3D CBCT imaging. The information is then merged and organized within the ALFRED digital platform, where it can then be viewed by the clinician along with other patient data such as medical history, extraoral examination, intraoral examination, photographs, and intraoral X-rays.
Integrating information into a single digital structure allows the clinician to gain in-depth knowledge of the patient and better respond to their needs and expectations. Specifically, it allows for the virtual implant-prosthetic design to be created with careful consideration of biomechanics: a biomechanically sustainable virtual design.
Therefore, the number, position, and dimensions of the implants (diameters and lengths), as well as abutments for screw-retained or cemented prostheses, are chosen in advance, always taking into account aesthetics and function. Last but not least, the presence of attached gingiva can be assessed and measured. Consequently, guided surgery with or without a flap is chosen. In particular, it is important to remember that flapless surgery represents an ideal solution for carefully selected cases with sufficient amounts of both bone and attached gingiva.
Thanks to the collaboration with Dr. Maurizio Monaco, we present the clinical case of an immediate temporary rehabilitation screwed with B1ONE monophasic implants and disparallelism compensators.
B1ONE combines the biomechanical strength of a single-stage implant with the versatility of a two-stage implant. The innovative connection allows the abutment-implant interface to be moved coronally, away from the bone tissue and ensuring undisturbed healing. Furthermore, the concave implant neck (STS-Soft Tissue Stabilizer) facilitates a minimally invasive surgical procedure and more space for soft tissue maturation.
When we encounter rehabilitations such as the following, with good bone availability and expectations of improved aesthetic and functional profile, it is important to study the most effective method to achieve it, where effectiveness means achieving the objectives with the least possible morbidity.
After a session to present the therapeutic options, digital information was acquired that allowed for precise and correct planning of the work to be carried out.
Figs. 1, 2 Initial clinical situation: frontal view and occlusal view, 3Shape Trios digital impression
Tooth extractions of all upper arch elements were performed and a temporary full-digital complete denture was delivered to promote tissue healing, restore the patient's chewing function and, at the same time, perform a preliminary aesthetic study to guide subsequent implant-prosthetic planning.
Fig. 3 Full-digital temporary total denture
Figs. 4, 5 Clinical situation after healing after extraction of all upper teeth: frontal view and occlusal view
The virtual design phase allowed us to position the implants in compliance with the available bone, to optimize the distribution of masticatory loads and to follow the diagnostic prosthetic wax-up.
Figs. 6, 7 Virtualization and planning for the guided surgery phase: matching between CBCT, intraoral scanning and diagnostic wax-up
In some anatomical areas, bone availability was lacking in the vestibular-palatal direction, which led to the choice of an implant that simultaneously met mechanical and morphological requirements without resorting to regenerative methods. Specifically, 3.2 mm diameter B1ONE implants were chosen, which were attached to larger diameter implants within the upper arch.
Figs. 8, 9. Planning the placement of 6 B1ONE implants to achieve biomechanically sustainable rehabilitation. The implants are selected based on the diameter, length, and geometry of the threads consistent with the quantity and quality of bone at the recipient site.
An assessment of the availability of keratinized tissue was then performed and a guided surgical technique without flap preparation was chosen. Following these indications, the template for the guided surgery procedure and the temporary restoration with metal framework were commissioned, which were manufactured by the IDI MAKERS digital dental technology department and sent to the office in the BLACKBOX.
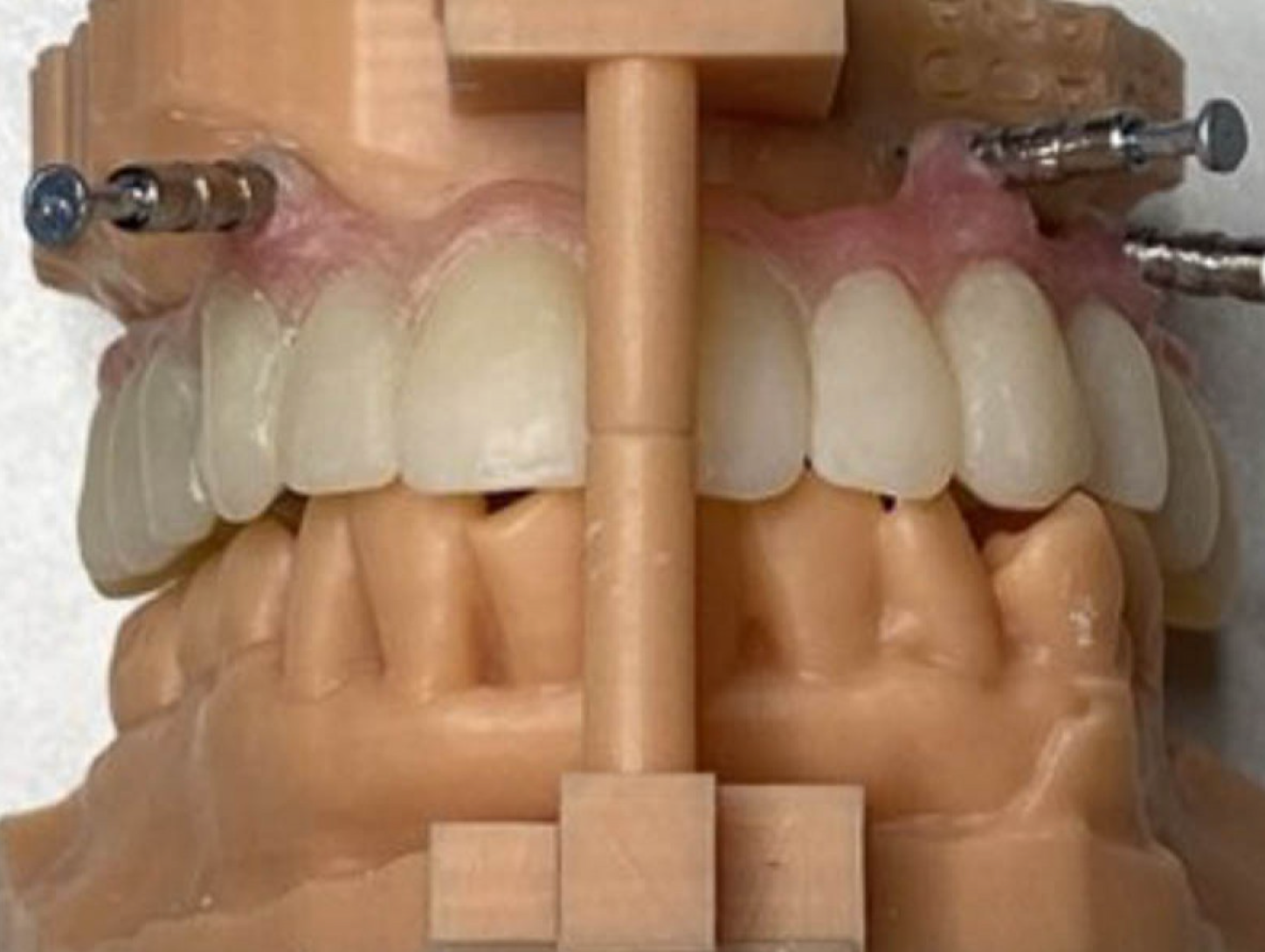
Figs. 10, 11 BLACKBOX by IDI EVOLUTION: model and surgical mask from digital workflow
Figs. 12, 13 BLACKBOX by IDI EVOLUTION: temporary prosthesis for immediate loading from digital workflow
The surgical phase was simple and minimally invasive and allowed for rapid positioning of the temporary restoration, which was passivated and bonded to the retained abutments.
Figs. 14, 15 Positioning of 6 B1ONE implants using the flapless guided surgery method: the patented, space-saving intacoronal connection allows for simple compensation of implant disparallelism, leaving room for the maturation of hard and soft tissues, guaranteeing stability, biomechanics and a seal against bacterial infiltration.
As easily predictable, the restoration of the dentition, in addition to an improvement in the quality of life, had an immediate effect on the patient's profile.
Figs. 16, 17 Long-term immediate loading temporary prosthesis made by the IDI MAKERS digital dental technology department of IDI EVOLUTION: intra-oral passivation and delivery to the patient
Figs. 18, 19. Patient profile: comparison between the start and end of implant-prosthetic therapy. An aesthetic improvement is evident, with restoration of the VDO, recovery of volume and exposure of the upper lip, and improvement of the nasal tip.
Fig. 20 Control orthopantomography 12 months after loading: long-term provisional
Work by Dr. Maurizio Monaco
Read the article on Odontoiatria33.























Share: