IMPLANT-PROSTHETIC SUCCESS COMES FROM DIGITALIZATION
Patients' clinical needs are increasingly focused on minimally invasive procedures, coupled with factors such as aesthetics, shorter treatment times, and cost savings. It's clear that these different needs, while legitimate, are difficult to reconcile.

In our work, we dentists must be able to meet all these needs, along with complying with various requests, the ever-increasing number of bureaucratic obligations, and the related increase in costs.
However, I would like to address the topic of the so-called " mirror test ," a moment that can be a harbinger of intense stress. The professional life of a dentist, implantologist, orthodontist, periodontist, and especially a prosthodontist, experiences intense emotional moments, for better or for worse, but there is a particular moment when the anticipation truly makes you hold your breath! Months of work, commitment, and study will be rewarded or thwarted in a matter of seconds.
It's the moment of truth, of judgment, the moment when we say we've finished our job and the patient asks the assistant... for the mirror!
It matters little whether you've performed complex surgical procedures with excellent results, or whether pre-existing clinical conditions would not have allowed for a better outcome: the patient sees only what the mirror reflects before their eyes and compares it to their more or less achievable expectations. And based on this, they will judge us and the work performed.
This can be a moment of joy, which turns into satisfaction and the desire to work even harder if the patient expresses happiness and gratitude, or a moment of disappointment that turns into a lack of motivation or anger if the patient doesn't appreciate the final result.
That's why we professionals We need to talk to the patient right away , before starting work, and set expectations realistically.
How can we do this if we haven't done a proper case study?
How can we answer questions about the possibility of fulfilling the patient's requests if we have not adequately assessed the clinical situation at hand?
I'd like to add a further consideration. Patient litigation has reached significant proportions. How can we limit problems, errors, and failures?
How can we always be able to defend our actions?
We can properly address all the above issues by dedicating much more time than in the past, at the programming and pre-operative prosthetic planning of the case and, in the case of implant-prosthesis, to a correct design of number, size and positioning in the various planes of space implant fixtures , designed to provide the best support for the planned prosthesis from a biomechanical point of view.
Ultimately, it is necessary to evaluate the soft tissues that must ensure the biological seal, and therefore the long-term clinical success, of our prosthetic rehabilitation. Furthermore, it is absolutely essential to maintain appropriate documentation of all these steps.
Prosthetics, in fact, plays a predominant role in rehabilitation. While years ago, surgeons would insert implants where bone volume permitted, leaving all the issues to the prosthetic surgeon, today, all surgical procedures must be performed with a precise prosthetic orientation, as well as with an eye to the biology and the varying load-bearing capacities of the jaw bone structures, because it is at this point that the outcome of the "game" is decided. That is, long before we begin our surgery.
Finally, the responsibilities of our profession. Today, immediate loading is advertised as if it were the norm, and only photos of that perfect job that happens once a year and involves no compromise whatsoever are posted on social media.
Advertising the exception as if it were the norm certainly doesn't help us. Because patients rightly demand that this exception be consistently implemented!
In short, today's dentists have significant disadvantages compared to their colleagues of the past; however, they also have two very important advantages that dentists of just 15-20 years ago did not have.
First and foremost , modern CT scans allow us to see the patient's anatomy like never before, in a 1:1 ratio and with incredible resolution. Our diagnosis, which represents the first and most important medical procedure, has never been so accurate in every branch of dentistry. We can have a 3D-printed model of the patient's jaw (instead of the old solid plaster model) on our desk and calmly evaluate every option before operating, even trying different simulations. Just a few years ago, surgeons were almost forced to improvise on the spot, with mixed results.
The second advantage we have today is linked to the advent of technology and, in particular, digital, which has truly revolutionized our entire world and the way we work.
Today, we can preview the final result . Not only is it a visualization of the planned work "fitted" into the patient's virtual dental arch, but thanks to facial scanners, we can also see the patient's new smile inserted into their face and obtain consent before starting our work.
Furthermore, the advent of software that simulates individual patient jaw movements allows us to create functionally valid prostheses, not because we prefer a particular tooth position or cusp-fossa or intermaxillary relationships, but because that tooth conformation, that positioning, those guides are what the patient needs to be comfortable, to avoid interference, to maintain the correct free space, and to avoid invasion of the lingual space.
These are no small advantages. Consider the prosthetic "touch-ups" that used to be done: how frustrating it was to destroy that beautiful cusp anatomy that our technician had painstakingly constructed, following the subjective "feel good and comfortable" of the patient as he dynamically attempted to articulate the dental arches together.
Unfortunately for us, those individual movements were not reproducible on any articulator; statically, the work seemed perfect, but in that patient's oral cavity, that beautiful work was "non-functional."
Therefore, a correct diagnosis, a prosthetic planning and an accurate implant design, using all the technology at our disposal , These are the premises for our prosthetic, aesthetic and functional success.
The cost impact, which does exist, must be managed by showing and explaining our analysis of "their" case to the patient, giving due importance to the time spent, which is the most precious thing we have, and the technology we will use. However, it is essential to show the patient, at least in major rehabilitation, what the final outcome of our work could be. This way, the patient will perceive the quality of what we are doing for them and will also better understand the costs.
Above all, we will obtain truly informed consent from the patient and will have no "negative surprises" during the mirror test, because everything will already be practically known and decided from the beginning of our work.
Clinical case presentation
To better explain the concepts expressed, we will now evaluate a relatively simple, but already indicative, case, with attention focused, in this first part of our work, on implant design.
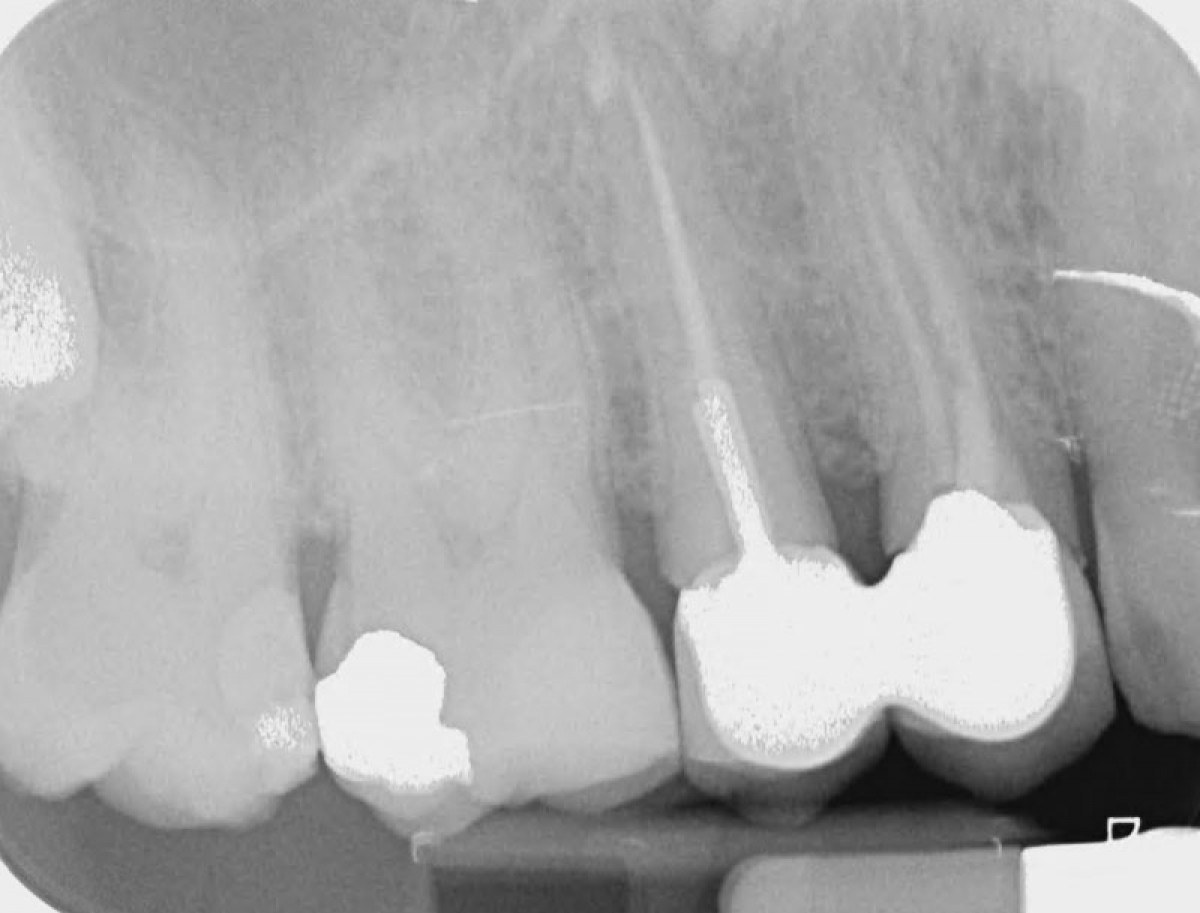
The patient being treated is a 61-year-old male with missing two premolars in the first quadrant (a fairly common condition for today's 60-70 year-olds, when the premolars had developed caries at a very young age); initially filled, then root canal treated and fitted with prosthetics, and finally affected by a root fracture/apical pathology, requiring extraction.
2015
2015
2022
As mentioned, the case is not complex, but it does present critical issues that should not be underestimated.
Let us remember:
- post-extraction site of fractured element;
- request for reduction of processing times;
- aesthetic area.
It is therefore essential to dedicate the appropriate amount of time to our planning, evaluating the various implant options after having, together with the patient, ruled out the traditional prosthetic option. This is because the teeth adjacent to the edentulous area are vital.
The decisions to be made after choosing early implant placement are, in order, the following.
1. Evaluation of prosthetic feasibility with a preview of aesthetics, prosthetic emergence, adequate hygienic maintenance options, and functionality of implant-supported, screw-retained, or cemented crowns, with the option of inserting various dedicated abutments into the software. It's clear that all these choices aren't based on our general or practical preferences.
2. Choice of the appropriate implant type to reduce the risk of failure and to allow good healing of hard and soft tissues.
3. Careful study, design, and planning of all surgical phases and procedures required to achieve the project.
It's understandable that the decision-making and operational dogma has been completely overturned. Just a few years ago, we would have had two implants, perhaps waiting a year after extraction, and then, once healing was complete, we would have addressed the prosthetic issue, assuming all the associated risks, especially for the aesthetic result, which today is essential.
The first diagnostic phase consists of a three-dimensional x-ray (TCCB) examination that allows for an accurate assessment of the treatment site. The native DICOM 3.0 files are imported into dedicated implant planning software. All our evaluations then begin in the order mentioned above.
The bone site must be considered in its three-dimensional volume, but also from the point of view of bone quality, keeping in mind the mineralization lost due to the infection caused by the vertical fracture.
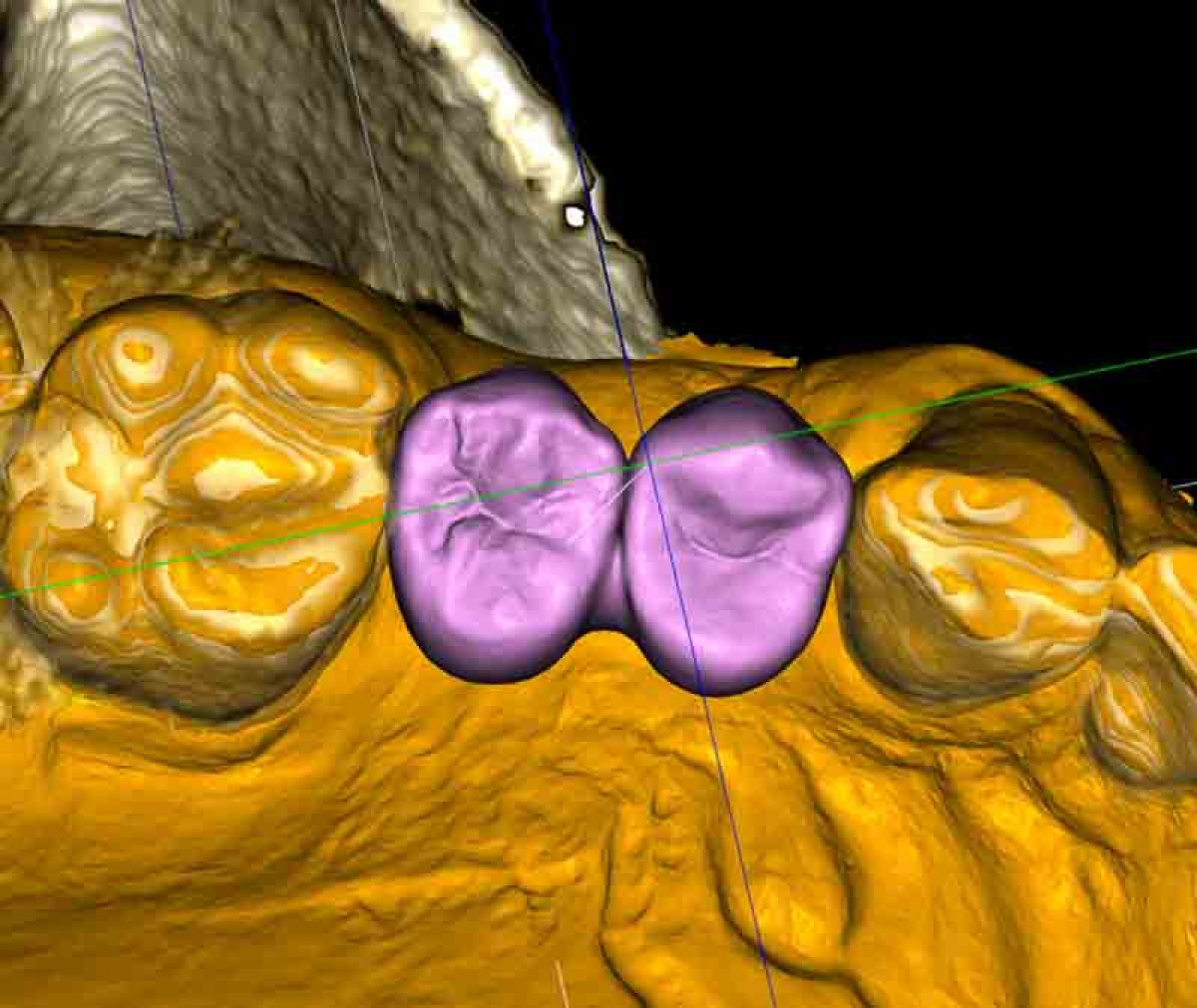
The intraoral scans acquired with the intraoral scanner are then aligned with the TCCB DICOM files.
The information we possess, at this point, is already relevant and much more in-depth than even in the recent past: space and inter-arch relationships, occlusal typology, the ability to visualize wear, junctions, guides, but above all the ability to aesthetically preview the final rehabilitation, with a very simple virtual diagnostic wax-up done on the software.
Virtual waxing is essential for correctly planning the implant position and inclination, in order to obtain an optimal emergence suitable for our prosthetic purposes.
The first diagnostic phase is followed by the choice of the implant type that we believe is optimal for the success of our therapy: which implant, which thread, which connection, which prosthetic components?
Already at the beginning of the 1990s, Carl E. Mish had hypothesized 3 different types of implant threads (Biohorizons, Maestro System) in order to obtain the best biomechanical performance in the different qualities of the bone tissue in the various areas of the jaws.
All his studies and work have been sacrificed for the convenience required by operators and for cost reduction, driven by the ruthless competition of the market. But a single implant, with a single thread, good for all "seasons" is not exactly what bone tissue requires.
Subsequent studies have thus focused primarily on surface treatment, which in our opinion is not so crucial. Ultimately, the possibility of reducing the time required to achieve osseointegration by 30 days does not seem so important to us for a therapy that must last for years.
We believe the study of the implant/abutment connection is much more important. This is the truly critical area, where all our peri-implant pathology problems arise.
The Italian B1ONE implant produced by IDI EVOLUTION was created to address these real clinical needs and has been able, in our opinion, to revolutionize the approach to the problems exposed.
The implant features the world's first intracoronal connection composed of a Torx-type anti-rotational system combined with a double cone. The underlying portion features a machined concave neck with reduced crestal bulk for maximum bone preservation and tissue stabilization. Finally, there are three types of threads for different bone qualities: High, Medium, and Low.
The surgeon therefore has the widest choice of threads and sizes in order to optimize load management capabilities, together with the best design for maintaining the crestal bone.
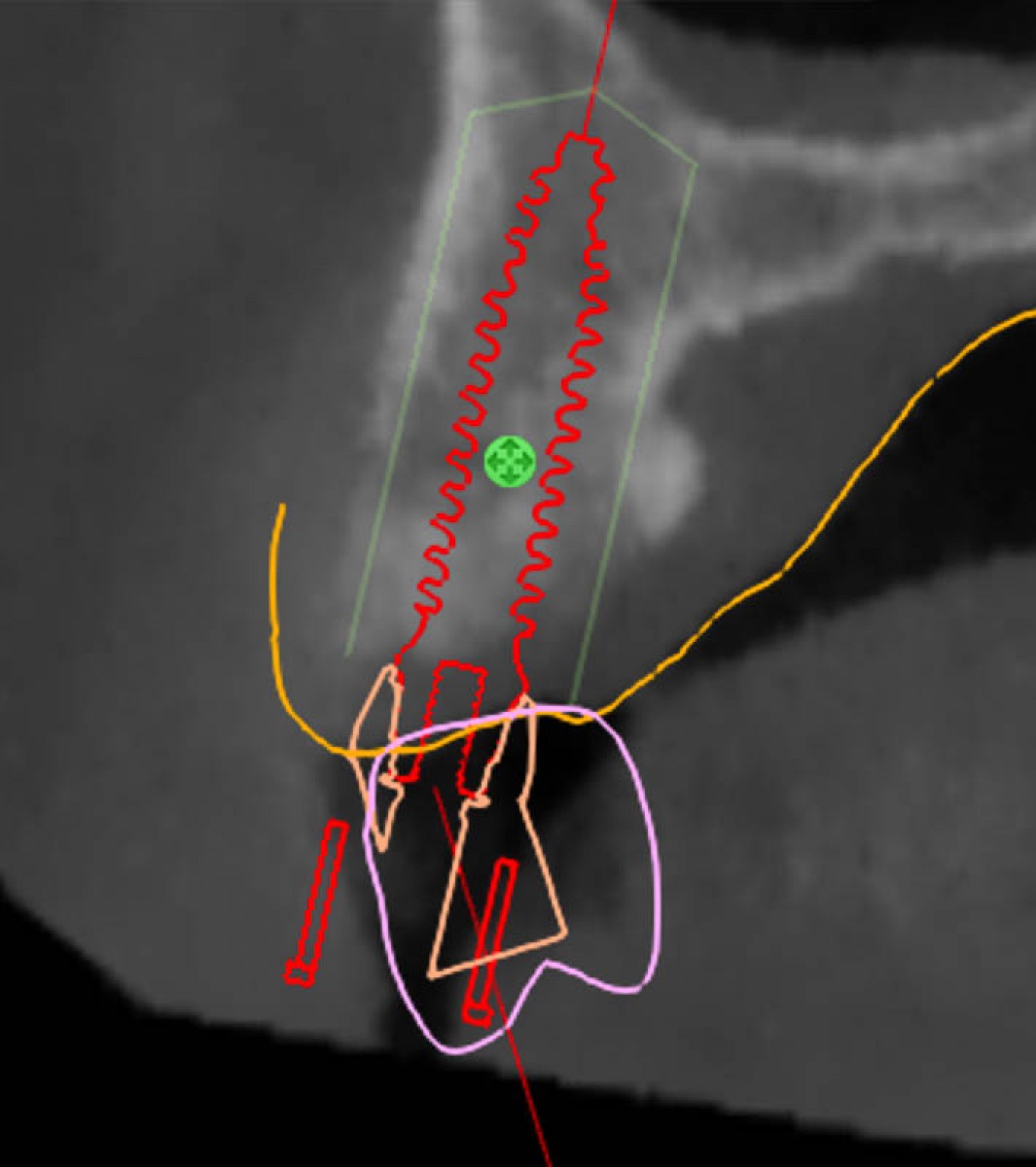
The final phase of our case study consists of implant planning.
One of the critical factors for the long-term success of our therapy is maintaining a correct inter-implant distance. This distance must be at least 3 mm (Tarnow, Cho, and Wallace, 2000) to maintain optimal vascularization of the inter-implant bony septum, a delicate area from a vascular perspective due to the loss of periodontal vessels and the septal arteriole following tooth extraction.
Implant planning software allows you to set the inter-implant clearance. Setting 1.5 mm around each implant allows you to respect the essential 3 mm. The software will highlight any critical selection issues in red.
Example with inter-implant safety zone not respected
Once we've decided on the implant type that we feel best guarantees crestal bone preservation even after prosthetic placement, this implant type must also allow us to choose the implant thread we deem most appropriate for that specific bone quality. In this case, the choice fell on the "Low" bone thread, designed for D4 bone.
To choose the right implant type and thread type, it's essential to correctly plan the implant placement. Simulation software is essential for performing various "positioning" tests, evaluating the potential final result achievable in terms of biomechanics, emergence and therefore aesthetics, hygiene options, and the relationship between implant fixtures and between implants and adjacent tooth roots.
Below are several simulations.
With angled implants
With implants in prosthetic axis
The implant axis should respect the biofunctionality of the coronal axis with proper vestibular-palatal balance. An excessively palatal positioning can cause periodontal problems due to hygiene difficulties; an excessively vestibular positioning can cause aesthetic defects due to crowns that are too long.
In this case, the horizontal dimension of the crest in the vestibular-palatal direction allows for both solutions; it will therefore be necessary to analyze all the information acquired during the examination, including the patient's aesthetic needs, and a discussion with the prosthetist to assess his or her preferences.
In any case, we have all the information we need to make the right decision and adequately plan our implant placement, which will be performed using a surgical drilling template. This will translate our virtual decisions into clinical reality, ensuring that the design is correctly, precisely, and extremely predictably implemented.
End of part one: the case will be completed in a new article from the Innovation Observatory.
We would like to thank Dr. Massimo Fagnani for his clinical and scientific contributions.
Read the article on Odontoiatria33.





















Share: